Publication links
Abstract
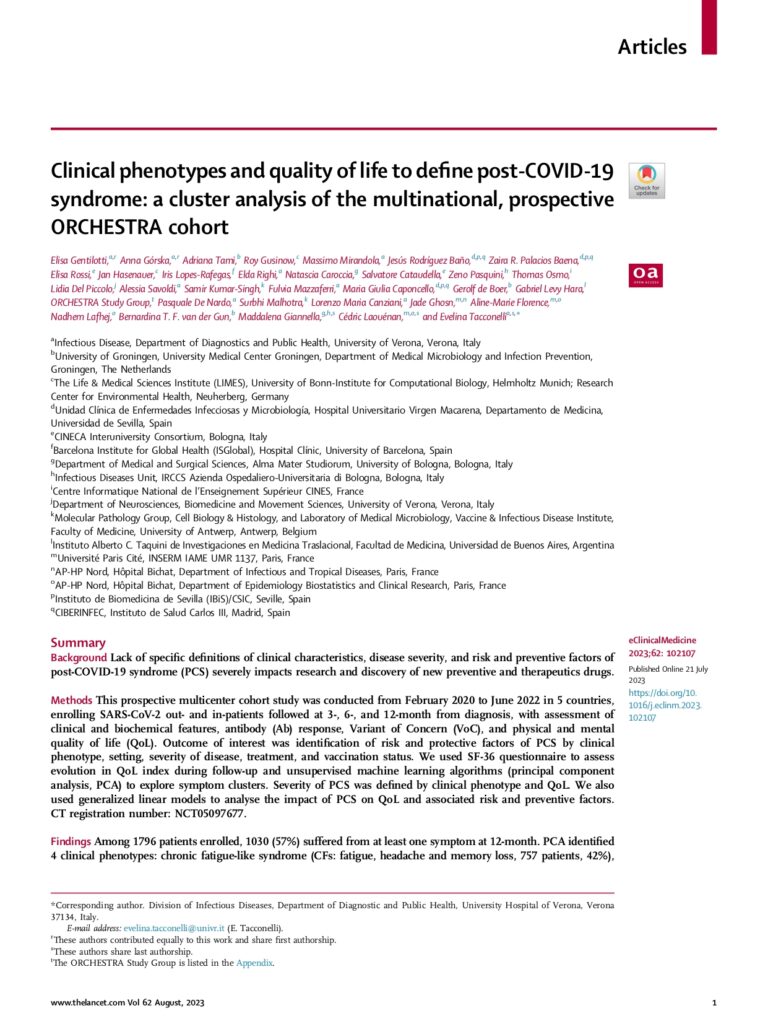
Background
Lack of specific definitions of clinical characteristics, disease severity, and risk and preventive factors of post-COVID-19 syndrome (PCS) severely impacts research and discovery of new preventive and therapeutics drugs.
Methods
This prospective multicenter cohort study was conducted from February 2020 to June 2022 in 5 countries, enrolling SARS-CoV-2 out- and in-patients followed at 3-, 6-, and 12-month from diagnosis, with assessment of clinical and biochemical features, antibody (Ab) response, Variant of Concern (VoC), and physical and mental quality of life (QoL). Outcome of interest was identification of risk and protective factors of PCS by clinical phenotype, setting, severity of disease, treatment, and vaccination status. We used SF-36 questionnaire to assess evolution in QoL index during follow-up and unsupervised machine learning algorithms (principal component analysis, PCA) to explore symptom clusters. Severity of PCS was defined by clinical phenotype and QoL. We also used generalized linear models to analyse the impact of PCS on QoL and associated risk and preventive factors. CT registration number: NCT05097677.
Findings
Among 1796 patients enrolled, 1030 (57%) suffered from at least one symptom at 12-month. PCA identified 4 clinical phenotypes: chronic fatigue-like syndrome (CFs: fatigue, headache and memory loss, 757 patients, 42%), respiratory syndrome (REs: cough and dyspnoea, 502, 23%); chronic pain syndrome (CPs: arthralgia and myalgia, 399, 22%); and neurosensorial syndrome (NSs: alteration in taste and smell, 197, 11%). Determinants of clinical phenotypes were different (all comparisons p < 0.05): being female increased risk of CPs, NSs, and CFs; chronic pulmonary diseases of REs; neurological symptoms at SARS-CoV-2 diagnosis of REs, NSs, and CFs; oxygen therapy of CFs and REs; and gastrointestinal symptoms at SARS-CoV-2 diagnosis of CFs. Early treatment of SARS-CoV-2 infection with monoclonal Ab (all clinical phenotypes), corticosteroids therapy for mild/severe cases (NSs), and SARS-CoV-2 vaccination (CPs) were less likely to be associated to PCS (all comparisons p < 0.05). Highest reduction in QoL was detected in REs and CPs (43.57 and 43.86 vs 57.32 in PCS-negative controls, p < 0.001). Female sex (p < 0.001), gastrointestinal symptoms (p = 0.034) and renal complications (p = 0.002) during the acute infection were likely to increase risk of severe PCS (QoL <50). Vaccination and early treatment with monoclonal Ab reduced the risk of severe PCS (p = 0.01 and p = 0.03, respectively).
Interpretation
Our study provides new evidence suggesting that PCS can be classified by clinical phenotypes with different impact on QoL, underlying possible different pathogenic mechanisms. We identified factors associated to each clinical phenotype and to severe PCS. These results might help in designing pathogenesis studies and in selecting high-risk patients for inclusion in therapeutic and management clinical trials.
Funding
The study received funding from the Horizon 2020 ORCHESTRA project, grant 101016167; from the Netherlands Organisation for Health Research and Development (ZonMw), grant 10430012010023; from Inserm, REACTing (REsearch & ACtion emergING infectious diseases) consortium and the French Ministry of Health, grant PHRC 20-0424.
Keywords
Citation
Gentilotti E, Górska A, Tami A, Gusinow R, Mirandola M, Rodríguez Baño J, Palacios Baena ZR, Rossi E, Hasenauer J, Lopes-Rafegas I, Righi E, Caroccia N, Cataudella S, Pasquini Z, Osmo T, Del Piccolo L, Savoldi A, Kumar-Singh S, Mazzaferri F, Caponcello MG, de Boer G, Hara GL; ORCHESTRA Study Group; De Nardo P, Malhotra S, Canziani LM, Ghosn J, Florence AM, Lafhej N, van der Gun BTF, Giannella M, Laouénan C, Tacconelli E. Clinical phenotypes and quality of life to define post-COVID-19 syndrome: a cluster analysis of the multinational, prospective ORCHESTRA cohort. EClinicalMedicine. 2023 Jul 21;62:102107. doi: 10.1016/j.eclinm.2023.102107. PMID: 37654668; PMCID: PMC10466236.